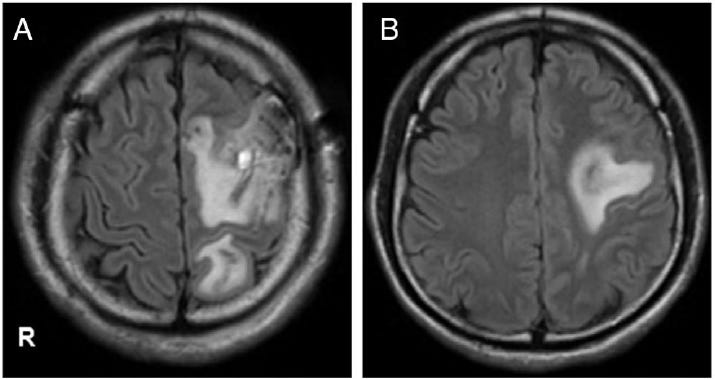
When I first came across a recent case report from Japan, I was struck by how it epitomized the challenges we face in understanding complex medical phenomena post-COVID-19. The case involved a 28-year-old man with central nervous system (CNS) vasculitis mimicking a brain tumor. What made it particularly compelling wasn’t just the rarity of the condition but the intricate web of questions it raised about immune responses, inflammation, and the long-term effects of viral and vaccine exposures.
This case embodies the very essence of my research into what I’ve termed the "COVID Storm" - the Spike Triggered Autoimmune Response Mechanism. It’s a concept I’ve developed to explain the cascading immune reactions that can arise following exposure to the spike protein, whether from the virus itself or vaccines.
The Role of Histology in Unraveling Complex Cases
One of the most striking aspects of this case was how elusive the diagnosis was. The patient’s blood tests were largely normal, with no clear indicators of systemic inflammation. Even cerebrospinal fluid analysis came back unremarkable. It wasn’t until a brain biopsy was performed that the true nature of the condition - ANCA-associated vasculitis - was revealed.
This underscores a critical point: without histology, we are often flying blind. Histological analysis - studying tissue under the microscope - is the gold standard for diagnosing conditions like vasculitis, where inflammation is localized to specific blood vessels. Without it, conditions like this one can go unnoticed or be misdiagnosed, leaving patients without answers.