Proposed risk stratification for severe COVID-19 in younger "healthy" individuals
Above is a summary of my understanding for risk of severe COVID-19 in the younger patient cohort. This piece of the puzzle was related to an important paper demonstrating the association with inflammatory bowel and severe COVID-19 disease.
The first principle is that nothing in medicine and science is random. There will always be a logical, scientific explanation for all patterns of disease. We just need to look thoroughly.
Myosin light chain 9 (Myl9) has been found to have elevated plasma levels in cases of inflammatory bowel disease.
Yokoyama, Masaya, et al. "Myosin light chain 9/12 regulates the pathogenesis of inflammatory bowel disease." Frontiers in Immunology 11 (2021): 594297.
This association is also followed in severe COVID-19. Additionally the Myl9 is deposited in the arteries of lung tissue with associated vasculitis.
In addition, the Myl9 level at admission was correlated with the duration of hospitalization and the risk of requiring oxygen supplementation at 7 d after administration. Thus, plasma Myl9 can be a useful biomarker to predict the future severity of COVID-19, and the measurement of Myl9 may allow us to detect patients with a high risk of becoming critically ill.
Iwamura, Chiaki, et al. "Elevated Myl9 reflects the Myl9-containing microthrombi in SARS-CoV-2–induced lung exudative vasculitis and predicts COVID-19 severity." Proceedings of the National Academy of Sciences 119.33 (2022): e2203437119.
Has this paper changed my perspective on the importance of serum ACE-2?
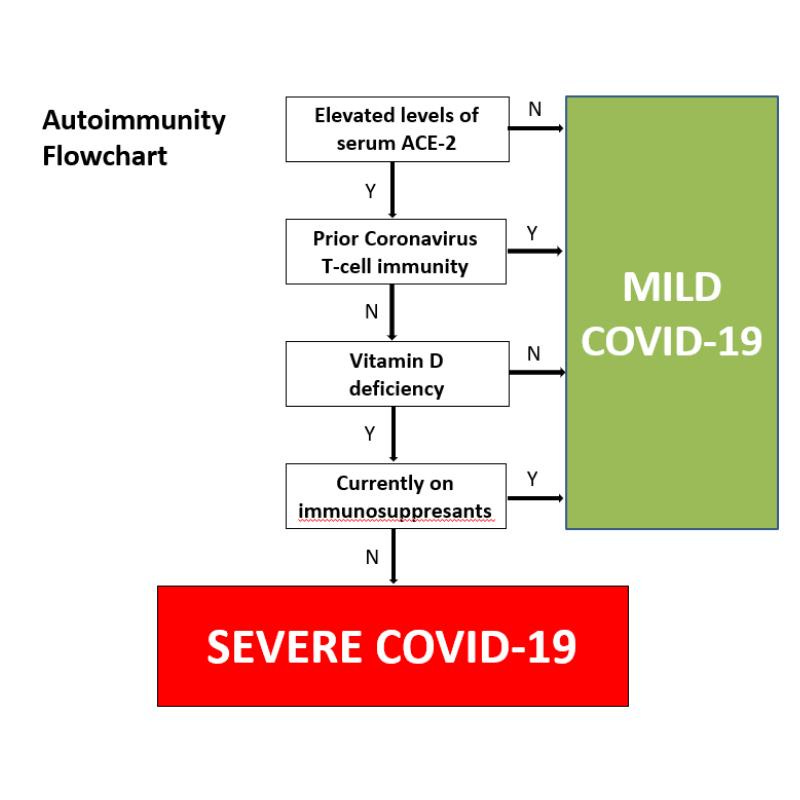
I have differentiated this from the older patients with elevated levels of serum ACE-2 as the primary driver for severe disease. Autoimmunity involving serum ACE-2 is the foundation of my research into severe COVID-19 being a viral mediated autoimmune disease. In reality there is an overlap as the older cohort will also have higher levels of inflammatory bowel disease. The below autoimmunity flowchart will also need some updates.
Many persons who are apparently “healthy” underestimate the impact of their diet on gut health. Subclinical inflammatory bowel disease is not to be underestimated.
Understanding the flowchart in short podcasts:
Can moderate/severe COVID-19 be defined?
What is Mucosal Immunity
How are interferon autoantibodies connected to severe COVID-19? What are the characteristics of those affected individuals?
Inflammatory bowel disease explained as a critical risk for severe COVID-19
Is immunosuppression beneficial for risk reduction?
What is the connection to severe disease and vitamin D deficiency?
Define moderate/severe COVID-19
Needing hospitalisation with oxygen whether or not ICU is required (severe disease).
What is upper airway mucosal immunity?
Prevents a virus or bacteria getting into the blood stream
Connection of interferon autoantibodies to severe COVID-19. What are the characteristics of affected individuals?
Inflammatory bowel disease and severe COVID-19.
Immunosuppression can be protective in severe COVID-19.
Why talk about vitamin D deficiency?
Thank you for listening and I hope you found this information helpful in understanding why some healthy individuals got severe COVID-19.



There are 3 areas only affected by Covid but those 3 areas are vital as they link with all biological systems of human body. Hence damage to them can damage other body systems.
The physiology of those 3 systems have currently the wrong science or incomplete and unknown scientific and biological properties.
The 3 areas are:-
1 Gas Exchange current gas exchange concepts diffusion/Fick's Law just wrong
2Endothelial layer
3Glycocalyx layer
2 and 3 are the blood vessel linings and young adults damaged by Covid have these areas damaged and really malfunctioning.
They 2 and 3 together are chemical transport systems with a shielding immunity against pathogens from exhaled CO2/H2O nanobubble foam which can destroy viruses and bacteria. Also they have a surrogate neural messaging and energy system
Ref
https://doi.org/10.1017/S0033583519000118ef Endothelial surface layer
and also ref on Damage Gas exchange
covid and Pulmonary Surfactant
https://doi.org/10.1017/qrd.2022.1
Work of Prof Barry Ninham and Prof Reines
But Gas exchange no longer damaged as surfactant not now effected by Omicron but it was with previous variant Covid virus. No 2 and 3 can be damaged though and function limited that gives rise to the young adult Long Covid
Do you think clinical or sub-clinical inflammatory bowel disease is the main driver of severe COVID-19 in obese patients?